3D Mammogram: Who Needs One, What to Expect and More

Mammograms have been an important screening and diagnostic method for years. Most people are familiar with them, but 3D mammograms are a little different. This guide will discuss what makes this imaging technique unique, who benefits most from it and what to expect during the scan.
What is a 3D mammogram?
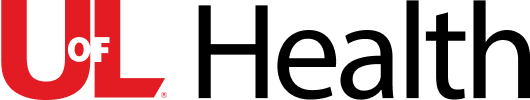
A simplified example of how a 3D mammogram image is built using many image slices taken at different angles, sourced from the National Cancer Institute via National Institutes of Health Image Gallery.
A mammogram is an X-ray that uses a very low radiation dose to examine breast tissue. These images can reveal any abnormal changes before they can be felt in a traditional breast exam.
In a 3D mammogram, the X-ray moves in an arc over the breast, taking multiple pictures from several different angles. Those images, called slices, are combined, providing a more complete view of the breast and making it easier to spot any irregularities. 3D mammograms are highly effective. A 2023 study of more than 1 million women showed that they led both to a higher rate of cancer detection and a lower rate of recalls for further imaging.
2D vs 3D mammograms: what is the difference?
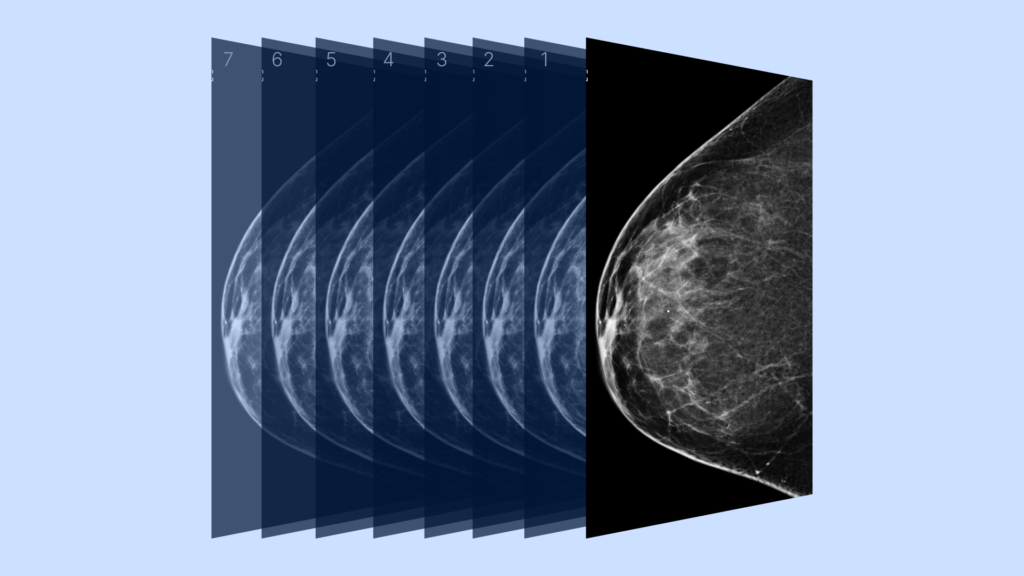
A 2D mammogram image
A traditional 2D mammogram provides 2 images of each breast (from the top and the side). 3D mammograms provide hundreds of thinly sliced images, which come together to create a highly detailed 3D view of the whole breast.
Mammograms are also the only way to assess breast density, which is important because dense breasts have increased cancer risks and can make abnormalities harder to spot. 3D mammograms are more effective for dense breasts because physicians can see the dense areas from several different angles.
A traditional 2D mammogram presents two overlapping images. That overlap can obscure potential abnormalities, causing them to be missed at the earliest stages. It’s also possible for overlapping tissue to make benign spots look abnormal, which then requires you to have further imaging done for clarification.
Who needs a 3D mammogram?
Some patients may benefit more from a 3D mammogram instead of a 2D one, especially if they have a higher risk of or history of breast cancer. Some advantages include:
- Increased accuracy: 3D mammograms detect the earliest signs of cancer at a higher rate than regular mammograms.
- Reduced need for follow-up imaging: The higher level of image clarity means fewer patients require follow-up scans.
- Effective for dense breasts: The fibrous nature of dense breasts makes it harder to see the early warning signs of cancer with a traditional 2D mammogram.
- Follow-up diagnostic screening: If you need a second scan, a 3D mammogram will provide more fine detail than a traditional mammogram.
Get early access to your mammogram results
How effective are 3D mammograms for breast cancer screening?
According to this 2023 study, 3D mammograms detect cancer in 5.3 out of 1000 cases, whereas traditional mammograms found cancer in 4.5 out of 1000. That’s a significant difference when it comes to early detection and treatment. Studies have also shown that 3D mammograms detect more kinds of cancer than regular 2D mammograms.
How often should you get a mammogram?
Medical bodies suggest different starting ages, but in 2023, the USPSTF issued a draft recommendation that women start regular screening mammograms every other year beginning at age 40. At 55, you can scan every year in the U.S.
Should you have a family health history of breast cancer, you should begin your screening sooner, and consider both mammograms and MRIs. Always discuss your risk factors with your physician so you can explore the best scan options for your particular needs.
PocketHealth recently launched breast health tools that provide patients with personalized breast cancer risk assessments and simplified mammogram management. Designed to increase early detection of breast cancer, these tools enable patients to take control of their breast health. Learn more about PocketHealth’s breast health tools here.

How to prepare for a 3D mammogram
While a 3D mammogram only requires a short appointment, there are some steps you can take to prepare. Here is a quick overview.
Preparations to make in advance
Ideally, you’ll want to make these preparations before your actual appointment.
- Schedule your mammogram when your breasts are least sensitive: They may feel tender leading up to or during your menstrual cycle, so consider not scheduling the scan within 7 to 10 days before your period.
- Use the same clinic: Whenever possible, have your mammograms at the same clinic each time. This will make it easier for the radiologist to compare images.
- Reduce caffeine intake: Caffeine can make breast tissue more tender, so try to avoid—or limit—caffeine intake for 4-5 days before your appointment.
- Let the clinic know if you have implants: Breast implants require modifications to the mammogram process, so your appointment may take longer. Also let the technologist know about any changes, sensitive areas or if you are breastfeeding.
- Let your doctor know if you have pain concerns: Getting a mammogram can be uncomfortable, as the breasts are compressed while the imaging is taken. If you are concerned about pain during your appointment, ask your doctor for recommendations.
- Obtain prior mammogram imaging: Consider obtaining or requesting imaging from previous mammogram clinics so that you have the imaging for your new appointment. PocketHealth helps you keep your medical imaging securely organized together, so you can bring them to your appointments yourself or share them at referral appointments. Having all your mammogram reports in one place lets you easily monitor imaging changes over time.
Preparations to make the day of your scan
Here are some day-of tips for your appointment:
- Bring your requisition: The requisition has important information for the imaging clinic or hospital. Also bring your health and I.D. cards.
- Avoid deodorant or antiperspirant and lotions: Don’t apply deodorant or antiperspirant on the day of your mammogram appointment, and make sure to wipe off any deodorant residue since the mammogram can pick up the aluminum. Also, avoid wearing powder or body lotion under your arms or your breasts. If you prefer, you can bring deodorant with you to apply after your appointment.
- Remove long earrings or necklaces: It’s best to avoid wearing jewelry to your appointment because the metal can interfere with your images.
- Wear a top and bottom, rather than a dress: You will be asked to remove your top and bra during your mammogram, so wearing pants or a skirt may make you more comfortable.
Pros and cons of 3D mammograms
As with all medical procedures, there are pros and cons when getting a 3D mammogram.
Pros
- Can detect more cancers
- Are more accurate when scanning dense breasts
- Provide a more complete picture of overall breast composition
- Result in fewer callbacks for further imaging
Cons
- Not every imaging clinic offers 3D mammograms
- Sometimes there is an extra cost that may not be covered by insurance
- Slightly longer exposure to low-dose radiation.
When will I get my 3D mammogram results?
Mammogram result turnaround times depend on the schedules of the radiologist and your doctor. They can take up to a week or more, especially if your doctor has scheduled a follow-up appointment to discuss your results. For patients wanting faster access, you can view your images and report through PocketHealth, often before your follow-up appointment.
PocketHealth allows you to access, view and store your medical images and health information all in one secure location. You can also use PocketHealth to share images, which is helpful if other medical providers need to review your mammograms.
Understanding your 3D mammogram results
Mammography reports are technical documents with complex terminology. PocketHealth Report Reader makes it easy to understand terms in your report and also highlights any follow-up recommendations, so you can be confident and informed when speaking to your doctor at your mammogram follow-up appointment.
Meanwhile, this guide will explain some of the conditions that mammograms scan for. While it can be easy to worry if you see these results in your report, just remember that it is very common for abnormalities to be benign. Your doctor will guide you on any additional testing or steps. Here are some helpful terms to know:
- Asymmetries: Areas that have a different shape than the surrounding breast tissue pattern. There are several types of asymmetry—in most cases, they do not represent cancer.
- Calcifications: Tiny deposits of calcium. Larger macro-calcifications are generally due to aging and don’t typically require a biopsy. Smaller micro-calcifications are more of a concern but do not in themselves indicate cancer.
- Distortions: These can be from a past injury or breast position on the X-ray table, but sudden significant distortion may require a follow-up diagnostic screening.
- Masses: An abnormal sector with distinct edges that look different from the surrounding breast tissue. Masses might indicate cancer, but they can also be fluid-filled cysts or non-cancerous fibroadenomas.
In a normal breast image, the background will be black while the breast tissue shows up in shades of gray. Dense tissue and glands will be white, whereas abnormalities like the ones listed above will have unique appearances. For example:
- Calcifications will be white flecks of varying size.
- Cysts will have thin walls and fluid-filled interiors.
- Cancer presents as a concentrated white area, like a tumor. However, most breast tumors are non-cancerous.
Some of these abnormalities will suggest further testing, which might include another mammogram or a biopsy.
Doctors use a standard vocabulary to describe mammogram results, called the Breast Imaging Reporting and Data System (BI-RADS). BI-RADS has 7 numbered categories:
- Category 0: Scan was incomplete or unclear, and you will need further testing or imaging for comparison.
- Category 1: A normal test result, considered ‘negative’ in that nothing abnormal or new was detected.
- Category 2: A normal test result, which includes some sort of non-cancerous finding like a benign calcification.
- Category 3: A possibly benign finding that suggests follow-up imaging, generally within the year.
- Category 4: A suspicious finding which is not confirmed to be cancer. A biopsy is often recommended.
- Category 5: These findings typically suggest cancer: a biopsy is strongly recommended.
- Category 6: This category is only used for findings taken after cancer has already been proven.
Take control of your breast health
Regular mammograms are vital for breast cancer detection and prevention. Mammograms of all types have life-saving potential since they can detect signs of breast cancer before you can feel them. Discuss 3D mammography with your physician to see if it’s the right choice for you. It’s important to stay both informed and proactive when it comes to maintaining your breast health.
PocketHealth provides great peace of mind for tracking your mammograms. For Mary, being able to review and compare her breast imaging led to the discovery that she was recommended to have these scans more frequently—something her primary doctor did not catch. Easy access to your mammogram records allows you to advocate for yourself, understand your needs and stay in control of your own breast health.
Published: September 5, 2023
Trusted by more than 800+ hospitals and clinics.